Abstract
Background:
Energy intake (EI) regulation is impaired in older adults, but it is not known if habitual physical activity affects accuracy of EI regulation in older compared with young adults.
Objective:
We hypothesized that the ability to compensate for a high-energy yogurt preload beverage at a subsequent ad libitum meal (i.e. acute compensation) and over the course of the testing day (i.e. short-term compensation) would decrease with age, but the magnitude of the decline would be smaller in physically active compared with sedentary older adults.
Design:
On two occasions, young active (n=15), young sedentary (n=14), older active (n=14) and older sedentary (n=11) subjects consumed either a high-energy yogurt preload beverage (YP: 500 ml, 1988 kJ, men; 375 ml, 1507 kJ, women), or no preload (NP), 30 min before an ad libitum test meal. EI at both ad libitum meals was measured, and total daily EI was determined on both testing days. Percent EI compensation for the YP was calculated for the test meal and testing day to determine acute and short-term compensation.
Results:
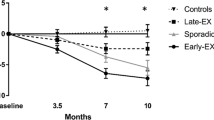
Percent EI compensation at the test meal was significantly lower in the older compared with the young subjects (65±4 vs 81±4%, P=0.005). There was no effect of habitual physical activity level on acute compensation, and no age by physical activity level interaction (P=0.60). In contrast, short-term compensation was not different with age (87±5 vs 93±6%, older vs young, P=0.45), but was more accurate in active vs sedentary subjects (100±5 vs 79±6%, P=0.01). As with acute compensation, there was no age by physical activity interaction (P=0.39).
Conclusion:
Acute EI regulation is impaired in older adults, which is not attenuated by physical activity status. However, EI regulation over the course of a day is more accurate in active vs sedentary adults, which may facilitate long-term energy balance. Future work is needed to determine if higher energy expenditure in older active vs older sedentary adults improves long-term EI regulation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM . Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006; 295: 1549–1555.
Arterburn DE, Crane PK, Sullivan SD . The coming epidemic of obesity in elderly Americans. J Am Geriatr Soc 2004; 52: 1907–1912.
Federal Interacency Forum on Aging Related Statistics. Older Americans 2004: Key Indicators of Well-Being ( http://www.agingstats.gov/chartbook2004/population.html#Indicator%201 ).
Roberts SB, Rosenberg I . Nutrition and aging: changes in the regulation of energy metabolism with aging. Physiol Rev 2006; 86: 651–667.
Rolls BJ, Dimeo KA, Shide DJ . Age-related impairments in the regulation of food intake. Am J Clin Nutr 1995; 62: 923–931.
Roberts SB, Fuss P, Heyman MB, Evans WJ, Tsay R, Rasmussen H et al. Control of food intake in older men. JAMA 1994; 272: 1601–1606.
Zandstra EH, Mathey MF, Graaf C, van Staveren WA . Short-term regulation of food intake in children, young adults and the elderly. Eur J Clin Nutr 2000; 54: 239–246.
Keene J, Hope T, Rogers PJ, Elliman NA . An investigation of satiety in ageing, dementia, and hyperphagia. Int J Eat Disord 1998; 23: 409–418.
Sturm K, Parker B, Wishart J, Feinle-Bisset C, Jones KL, Chapman I et al. Energy intake and appetite are related to antral area in healthy young and older subjects. Am J Clin Nutr 2004; 80: 656–667.
Long SJ, Hart K, Morgan LM . The ability of habitual exercise to influence appetite and food intake in response to high- and low-energy preloads in man. Br J Nutr 2002; 87: 517–523.
Blundell JE, Stubbs RJ, Hughes DA, Whybrow S, King NA . Cross talk between physical activity and appetite control: does physical activity stimulate appetite? Proc Nutr Soc 2003; 62: 651–661.
Stunkard AJ, Messick S . The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res 1985; 29: 71–83.
Radloff L . The CES-D scale: a self-report depression scale for research in the general population. Appl Psych Meas 1977; 1: 385–401.
Garner DM, Olmsted MP, Bohr Y, Garfinkel PE . The eating attitudes test: psychometric features and clinical correlates. Psychol Med 1982; 12: 871–878.
Institute of Medicine Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). The National Academies Press: Washington, DC, 2002.
Anderson GH, Catherine NL, Woodend DM, Wolever TM . Inverse association between the effect of carbohydrates on blood glucose and subsequent short-term food intake in young men. Am J Clin Nutr 2002; 76: 1023–1030.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Tsuchiya A, Almiron-Roig E, Lluch A, Guyonnet D, Drewnowski A . Higher satiety ratings following yogurt consumption relative to fruit drink or dairy fruit drink. J Am Diet Assoc 2006; 106: 550–557.
Rolls BJ, McDermott TM . Effects of age on sensory-specific satiety. Am J Clin Nutr 1991; 54: 988–996.
Rolls BJ, Kim S, McNelis AL, Fischman MW, Foltin RW, Moran TH . Time course of effects of preloads high in fat or carbohydrate on food intake and hunger ratings in humans. Am J Physiol Regul Integr Comp Physiol 1991; 260: R756–R763.
Porrini M, Crovetti R, Testolin G, Silva S . Evaluation of satiety sensations and food intake after different preloads. Appetite 1995; 25: 17–30.
Flint A, Raben A, Blundell JE, Astrup A . Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in single test meal studies. Int J Obes Relat Metab Disord 2000; 24: 38–48.
Parker BA, Sturm K, MacIntosh CG, Feinle C, Horowitz M, Chapman IM . Relation between food intake and visual analogue scale ratings of appetite and other sensations in healthy older and young subjects. Eur J Clin Nutr 2004; 58: 212–218.
Buffenstein R, Poppitt SD, McDevitt RM, Prentice AM . Food intake and the menstrual cycle: a retrospective analysis, with implications for appetite research. Physiol Behav 1995; 58: 1067–1077.
Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH . Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology 2003; 28: 916–931.
Villareal DT, Apovian CM, Kushner RF, Klein S . Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res 2005; 13: 1849–1863.
Villareal DT, Banks M, Sinacore DR, Siener C, Klein S . Effect of weight loss and exercise on frailty in obese older adults. Arch Intern Med 2006; 166: 860–866.
American College of Sports Medicine Position Stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 1998; 30: 992–1008.
Weinsier RL, Hunter GR, Desmond RA, Byrne NM, Zuckerman PA, Darnell BE . Free-living activity energy expenditure in women successful and unsuccessful at maintaining a normal body weight. Am J Clin Nutr 2002; 75: 499–504.
DiPietro L, Kohl III HW, Barlow CE, Blair SN . Improvements in cardiorespiratory fitness attenuate age-related weight gain in healthy men and women: the Aerobics Center Longitudinal Study. Int J Obes Relat Metab Disord 1998; 22: 55–62.
Manini TM, Everhart JE, Patel KV, Schoeller DA, Colbert LH, Visser M et al. Daily activity energy expenditure and mortality among older adults. JAMA 2006; 296: 171–179.
Acknowledgements
This work was supported by the Virginia Tech/University of Virginia/Carilion Biomedical Institute Collaborative Research Grants Program.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Walleghen, E., Orr, J., Gentile, C. et al. Habitual physical activity differentially affects acute and short-term energy intake regulation in young and older adults. Int J Obes 31, 1277–1285 (2007). https://doi.org/10.1038/sj.ijo.0803579
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803579
Keywords
This article is cited by
-
Association of Exercise with Control of Eating and Energy Intake
Current Addiction Reports (2019)
-
Issues in Measuring and Interpreting Human Appetite (Satiety/Satiation) and Its Contribution to Obesity
Current Obesity Reports (2019)
-
Impact of physical activity level and dietary fat content on passive overconsumption of energy in non-obese adults
International Journal of Behavioral Nutrition and Physical Activity (2017)
-
Does Habitual Physical Activity Increase the Sensitivity of the Appetite Control System? A Systematic Review
Sports Medicine (2016)
-
Homeostatic and Circadian Control of Food Intake: Clinical Strategies to Prevent Overconsumption
Current Obesity Reports (2013)