Abstract
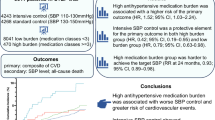
We assessed, in a double-blind, placebo-controlled trial, whether lowering blood pressure (BP) prevents the recurrence of stroke in Chinese patients with cerebrovascular disease. Patients were randomized into two groups: 2825 patients received a placebo and 2840 patients received 2.5 mg of indapamide daily. The primary and secondary outcomes were the recurrence of fatal or nonfatal stroke and major fatal and nonfatal cardiovascular events, respectively. The average systolic/diastolic BP at randomization was 153.8/92.8 mm Hg. At median follow-up (2 years), BP was, on an average, 6.8/3.3 mm Hg lower in patients on active treatment. In total, 143 patients on indapamide and 219 patients on placebo had recurrent strokes (hazard ratio for indapamide, 0.69; 95% confidence interval (CI): 0.54–0.89; P<0.001). In addition, 199 patients on indapamide and 258 patients on placebo had a cardiovascular event (hazard ratio, 0.75; 95% CI: 0.89–0.62; P=0.002). We performed a systematic review of literature that included our new results. Across 10 trials, the odds ratio for the prevention of stroke recurrence by BP lowering was 0.78 (95% CI: 0.68–0.90; P=0.0007). The pooled odds ratio was 0.63 (95% CI: 0.54–0.73; P<0.0001) for trials involving diuretics as a component of therapy and 0.93 (95% CI: 0.87–1.01; P=0.086) for trials in which treatment included renin system inhibitors (P<0.0001 for heterogeneity). The weighted correlation between the odds for stroke recurrence and the reduction in systolic BP was −0.57 (P=0.067). In conclusion, BP lowering by indapamide treatment reduced the recurrence of stroke and the incidence of cardiovascular events in Chinese patients with cerebrovascular disease. Whether prevention of stroke recurrence depends on drug class, degree of BP lowering or both requires further investigation.
Similar content being viewed by others
Introduction
The double-blind Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial involved 20 332 patients with ischemic stroke.1 Compared with placebo, the drug telmisartan reduced systolic/diastolic blood pressure by 3.8/2.0 mm Hg, but did not affect the incidence of recurrent stroke. The hazard ratio for this study was 0.94 (95% confidence interval (CI): 0.87–1.04; P=0.23). The PRoFESS trial showed that the addition of an angiotensin receptor blocker to existing antihypertensive drug treatment soon after stroke (within 10 days in 39.8% of randomized patients), and continued thereafter for 2.5 years, did not significantly reduce the risk of subsequent stroke.
The PRoFESS trial included 6660 Asians (32.8%), of whom 3666 (18.0%) were Chinese.1 The Post-stroke Antihypertensive Treatment Study (PATS) was a double-blind trial of blood pressure lowering by treatment with indapamide vs. placebo for the prevention of stroke recurrence in Chinese patients.2 The PATS trial was stopped prematurely in June 1994 because of a 29% decrease in the recurrence of combined fatal and nonfatal strokes.2 A preliminary report was published in 1995.2 In view of the inconclusive PRoFESS results,1 we reanalyzed the results of the PATS trial.2 Furthermore, we interpreted the results of this trial in Chinese patients2 within the framework of all available evidence from previous randomized clinical trials in patients with a history of cerebrovascular disease.1, 2, 3, 4, 5, 6, 7, 8, 9, 10
Methods
The PATS study
The goal of the PATS trial was to determine the effects of blood pressure lowering on the risk of stroke and other major vascular events in individuals with a history of stroke or transient ischemic attack (TIA). The Ethics Committees of the Fu Wai Hospital (Peking Union Medical College and Chinese Academy of Medical Science, Beijing, China) and of each participating center (see the Appendix) approved the protocol used. The principles outlined in the Helsinki Declaration were applied. Patients provided informed consent.
A total of 44 centers across China recruited patients, and each center maintained a register of screened patients. Patients with a history of TIA or minor stroke and those with a history of major stroke who were not severely disabled were eligible for the trial, irrespective of their blood pressure level and stroke subtype. The time interval between the qualifying cerebrovascular event and enrollment was ⩾4 weeks. Patients had to be clinically and neurologically stable without contraindications or compelling indications for blood-pressure-lowering treatment and had to be available for long-term follow-up. The exclusion criteria included secondary hypertension, malignancy, rheumatic valvular disease, heart failure, atrial fibrillation, hyperthyroidism, concurrent hepatic or renal diseases, hemorrhagic disorders and insulin-dependent diabetes mellitus.
Before randomization, potentially eligible patients participated in a 2-week run-in period, during which they took a placebo tablet in a single-blind manner. During two separate clinic visits in the second week of the run-in period, patients had their blood pressures measured twice after they had rested in a sitting position for at least 5 min. The baseline blood pressure was taken as the mean of these four readings. The last run-in visit also included an interview to obtain information on the patient's medical history and activities of daily living (ADL) and a physical examination and an ECG.
The Coordinating Center at the Fu Wai hospital generated a randomization list for each center. This list assigned patients to a batch of study medications to be taken after entry into the trial. Each bottle of study medication carried a unique identification number. Randomization was balanced within each center. The Coordinating Center also provided each center with sealed envelopes with the randomization code of each patient for use in case of an emergency, which necessitated breaking the code. After randomization, patients were started, in a double-blind manner, on 2.5 mg per day of indapamide or the corresponding placebo. All 3-monthly follow-up visits included an assessment of drug intake, adverse effects and possible events,2 measurements of sitting blood pressure and a count of the sitting pulse rate. The last follow-up visit also included an assessment of the ADL score and an ECG. Investigators immediately reported severe adverse events to the Coordination Office. To allow for an intention-to-treat analysis, patients who stopped taking the study medication on advice from their doctors, or patients who voluntarily withdrew from the double-blind trial, continued to remain in follow-up at the clinics on an annual or shorter interval basis (supervised open follow-up). If regular follow-up at the clinics was impossible, investigators annually updated information on the patient's vital status and the incidence of events through registries, hospital records or contacts with patients or their relatives in writing or over the telephone. Patients without any follow-up within the year before the trial stopped were considered lost to follow-up.
The primary end point was the recurrence of fatal or nonfatal stroke (International Code of Diseases (ICD-9, 1975) 430–434 or 436). A stroke is an acute disturbance in focal or global cerebral functions lasting ⩾24 h, which may lead to death, with no apparent cause other than vascular. Stroke does not include TIA, which is a focal cerebral dysfunction lasting <24 h. The secondary end points included sudden or rapid cardiac death, myocardial infarction, retinal hemorrhage, exudates or papilledema (stage III–IV retinopathy according to Keith–Wagener's classification), congestive heart failure (requiring the use of diuretics, vasodilators or any antihypertensive drug for a period longer than 3 months), enlarging or dissecting aortic aneurysms and the development of renal insufficiency (serum creatinine ⩾360 μmol l−1 (⩾4.0 mg ml−1)). Cardiac deaths were classified as sudden or rapid depending on whether death occurred within 1 or 1–24 h, respectively, after the onset of cardiac symptoms. A diagnosis of myocardial infarction required that at least 2 of the following three criteria were met: (1) chest pain lasting for at least 30 min, not responsive to nitrates, and presenting with or without irradiation of pain to the shoulder, arms, jaw or abdomen; (2) electrocardiographic changes characteristic of myocardial infarction (Minnesota codes 1-2-1, 1-2-2, 1-2-3, 1-2-6, 1-3-1 through 1-3-6, 2-4, 4-0, 4-1, 5-1); and (3) an increase in serum levels of alanine aminotransferase (within 72 h after the onset of symptoms) and lactate dehydrogenase (within 14 days after the onset of symptoms) to twice the upper limit of normal. At the time of the PATS trial, measurements of creatinine phosphokinase levels were not routinely available in China. An Endpoint Committee, blinded to the randomization of patients, reviewed the clinical records and adjudicated all primary and secondary end points.
Assuming a rate of stroke recurrence of 50 events per 1000 patient-years and a dropout rate of <30%, 5000 patients (2500 per treatment group), followed-up for 2 years, were sufficient to detect a 25% difference in stroke recurrence with a two-tailed significance of 1% and 90% power. We expected 500 strokes to occur in our patients within 2 years. We planned interim analyses after every 100 strokes to test for beneficial or adverse events occurring before the end of the trial. Asymmetrical monitoring boundaries, drawn according to the O'Brien–Fleming method, allowed us to terminate the study if we observed beneficial effects of active treatment on total stroke at 1% probability (adjusted for multiple looks at the data) or if we observed adverse effects of any major end point at 5%. At the third interim analysis in June 1994, we found a significant decrease in the occurrence of stroke in the active treatment group, which, based on the predefined rules for terminating the study, led to early termination of the trial.
We compared means, medians and proportions using the large-sample z-test, Wilcoxon's test and χ2 analysis, respectively, and we analyzed survival curves using Kaplan–Meier survival function estimates and the log-rank test. The effects of treatment on the risk of fatal and nonfatal stroke were also estimated using unadjusted Cox's proportional hazards models. To adequately represent relative risk reductions, we used the following formula: hazard ratio ([relative ratio−1] × 100). For participants who had more than one event within the same category during follow-up, only the first event was used for analysis.
Meta-analysis of blood-pressure-lowering treatment for the prevention of stroke recurrence
Ten randomized controlled trials1, 2, 3, 4, 5, 6, 7, 8, 9, 10 were performed to determine the effects of antihypertensive drug treatment vs. no treatment or placebo on recurrent stroke in hypertensive or normotensive patients with a previous history of cerebrovascular disease. We extracted the characteristics of the 10 trials and those of the patients enrolled in the trials who had a history of stroke from specific publications on stroke recurrence1, 2, 3, 4, 5, 6, 7, 8, 9, 10 or from articles describing the baseline data11 or main results12, 13 of the reviewed trials. We combined the results of the 10 trials1, 2, 3, 4, 5, 6, 7, 8, 9, 10 on the secondary prevention of stroke (11 groups of randomized patients) in stratified 2 × 2 tables. We computed pooled odds ratios from fixed-effects models or, in the case of significant heterogeneity, from random-effects models. In subgroup analyses, we contrasted trials that used a diuretic2, 3, 4, 7 as opposed to renin system inhibitors1, 5, 6, 7, 8, 9 as the main form of active treatment. Renin system inhibitors, in addition to angiotensin-converting enzyme inhibitors and angiotensin II type 1 receptor blockers, also included β-blockers.14, 15
We used the PROC MIXED procedure as implemented in SAS package (version 9.1.3; SAS Institute, Cary, NC, USA). We weighted pooled estimates of odds ratios by the inverse of the variance of the odds ratios in individual studies, and pooled estimates of the gradients in blood pressure by the number of patients randomized in each trial. We computed the weighted correlation between the odds of stroke recurrence on active treatment and the gradient in systolic blood pressure (active treatment minus control) randomized in the 10 trials.1, 2, 3, 4, 5, 6, 7, 8, 9, 10
Results
Stroke recurrence in the PATS trial
Of the 6645 patients who were screened during the run-in period, 5665 (85.3%) were randomized (Figure 1). At the time of randomization, patients in both the placebo (n=2825) and active treatment (n=2840) groups were similar in the distributions of sex, age, blood pressure, pulse rate, ADL score, type of qualifying cerebrovascular event and the time interval between the qualifying event and randomization (Table 1).
Patients were recruited over 3 years. The median follow-up time was 24 months (range, 0–45). The numbers of patient-years in the placebo and active treatment groups were 4967 and 5152, respectively. Figure 1 shows the status of all patients in June 1994 when the trial was prematurely terminated. After 2 years, during the intention-to-treat analysis, sitting systolic and diastolic blood pressures had fallen by an average (±s.d.) of 6.7±30.1 and 5.8±16.8 mm Hg, respectively, in the placebo group and by 12.6±30.5 and 8.9±16.4 mm Hg, respectively, in the indapamide group (Figure 2). At median follow-up, 24.9% of patients in the placebo group and 36.5% in the indapamide group had reached a blood pressure level of <140 mm Hg systolic and <90 mm Hg diastolic (P<0.001 for between-group difference). We calculated the differences in achieved blood pressure between groups by subtracting the changes from baseline in the placebo group from the corresponding changes in the indapamide group. For sitting blood pressure, the mean between-group difference was 6.8 mm Hg (95% CI: 5.3–8.3) systolic and 3.3 mm Hg (95% CI: 2.4–4.1) diastolic after 2 years and 5.9 mm Hg (95% CI: 3.6–8.3) and 1.7 mm Hg (95% CI: 0.4–3.0) after 3 years, respectively.
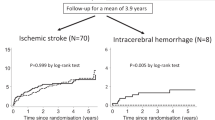
In addition, there were fewer deaths from stroke in the indapamide group (−26%; 95% CI: −47 to 3; P=0.07) than in the placebo group (Table 2). The between-group difference in total mortality and death rates due to cardiovascular causes, myocardial infarction, other cardiovascular disorders and noncardiovascular diseases did not approach significance (P⩾0.17; Table 2). The primary end point was the recurrence of fatal and nonfatal strokes. In both the placebo and indapamide groups, 219 and 159 patients experienced stroke recurrence with cumulative rates of 44.1 and 30.9 strokes, respectively, per 1000 patient-years (Table 3). The Kaplan–Meier survival function estimates started to diverge early in the trial (Figure 3). Indapamide (Table 3) reduced the recurrence of all strokes by 30% (P<0.001) and that of nonfatal strokes by 31% (P=0.005). The absolute reduction in the 3-year risk of stroke was 40 events per 1000 participants (95% CI: 18–62). In the indapamide group, all nonfatal cardiovascular end points, including stroke, myocardial infarction and other cardiovascular events, decreased by 31% (P=0.002). Active treatment reduced all fatal and nonfatal cardiovascular events by 25% (P=0.002).
Subgroup analyses of the primary end point (combined fatal and nonfatal strokes) did not show any heterogeneity in treatment effects based on sex, median age (60 years), blood pressure status at randomization, subtype of qualifying cerebrovascular event and the time interval between the qualifying event and randomization (Table 4). However, the power to detect heterogeneity was low. For example, considering a two-sided α-level of 0.05, the PATS trial only had 43% power to detect a 0.40 sex difference in the log hazard ratio for the effect of treatment on stroke recurrence.
Blood-pressure-lowering treatment in the prevention of stroke recurrence
Table 5 summarizes the main characteristics of the 10 reviewed trials on stroke recurrence1, 2, 3, 4, 5, 6, 7, 8, 9, 10 and those of the patients included in the meta-analysis. We combined the results of these 10 trials1, 2, 3, 4, 5, 6, 7, 8, 9, 10 (Figure 4). Overall, the odds ratio for the prevention of stroke recurrence due to blood-pressure-lowering therapy was 0.78 (95% CI: 0.68–0.90; P=0.0007). The pooled odds ratio was 0.63 (95% CI: 0.54–0.73; P<0.0001) for trials involving a diuretic as a component of experimental therapy2, 3, 4, 7 and 0.93 (95% CI: 0.87–1.01; P=0.086) for trials1, 5, 6, 7, 8, 9 in which the main form of treatment consisted of the renin system inhibitors atenolol,5, 6 perindopril,7 ramipril,8 candesartan9 or telmisartan.1 The P-value for the heterogeneity between studies involving diuretics vs. renin system inhibitors was <0.0001. In addition, there also was heterogeneity in the odds ratios between all trials (P<0.0001; Figure 4).
Effects of blood pressure lowering on fatal and non-fatal recurrent strokes. Solid squares represent the odds ratios of individual trials, and their sizes are proportional to the inverse of the variance. Horizontal lines and diamonds denote the 95% confidence intervals for individual trials and summary statistics, respectively. Pooled odds ratios were computed from a fixed-effect model, in the case of significant heterogeneity from a random-effect model. The vertical dotted line marks the position of the point estimate of the pooled effect size for all trials combined. TIA indicates transient ischemic attack. BP and ΔBP stand for the average blood pressure at randomization and the difference in achieved blood pressure between randomized groups, respectively. Pooled estimates of the gradients in blood pressure were weighted by the number of patients randomized in each trial. The individual studies were Carter's trial; the Hypertension-Stroke Cooperative Study (HSCS); the Dutch TIA Trial; the TEnormin after Stroke Trial (TEST); the Post-stroke Antihypertensive Treatment Study (PATS); the Perindopril PrOtection Against Recurrent Stroke Study—monotherapy (PROGRESS/Per) and combined therapy (PROGRESS/Com) arms; the Heart Outcomes Prevention Evaluation study (HOPE); Study on COgnition and Prognosis in the Elderly (SCOPE); the Felodipine EVEnt Reduction (FEVER) study; and the Prevention Regimen For Effectively avoiding Second Strokes (PRoFESS) trial. For Carter's trial, blood pressure at randomization was estimated by adding 10 and 5 mm Hg to the qualifying systolic and diastolic levels, respectively, at entry.
In the four trials that investigated the use of diuretics, administered alone (PATS) or in combination with anti-adrenergic agents3, 4 or perindopril,7 the average decrease in blood pressure was 8.5 mm Hg systolic and 3.6 mm Hg diastolic. In the six studies investigating the use of renin system inhibitors,1, 5, 6, 7, 8, 9 which were usually administered in addition to background treatment, the average decrease in blood pressure was 4.0 mm Hg systolic and 2.1 mm Hg diastolic. In all the studies combined,1, 2, 3, 4, 5, 6, 7, 8, 9, 10 the average reduction in blood pressure was 5.1 mm Hg systolic and 2.5 mm Hg diastolic (Figure 4). In weighted regression analysis, the correlation between the odds of stroke recurrence and the reduction in systolic blood pressure approached significance. The correlation coefficient was −0.58 (P=0.081) across 10 groups and −0.57 (P=0.067) when, for Carter's trial, a reduction of 10 mm Hg in systolic blood pressure was imputed to active treatment (11 groups).
Discussion
This analyses consolidate the preliminary results of the PATS trial published as a short report in the Chinese Medical Journal in 1995.2 In Chinese patients with a history of cerebrovascular disease, antihypertensive treatment with the sulfonamide diuretic indapamide16 at a daily dose of 2.5 mg lowered blood pressure by 6.8 mm Hg systolic and 3.3 mm Hg diastolic and reduced the incidence of stroke recurrence and combined fatal and nonfatal cardiovascular end points by 31 and 25%, respectively. These effects were consistent, irrespective of sex, median age, blood pressure status at randomization and subtype of the qualifying cerebrovascular event.
The PATS was the first randomized clinical trial in China designed and carried out according to the paradigm of a large-scale simple study.17 It was an investigator-initiated and investigator-led clinical trial with little funding. We used indapamide16, 18 because in the early 1990s this diuretic was one of the most commonly used generic antihypertensive drugs in China and also because it was very inexpensive. The Tientsin Lisheng Pharmaceutical Company (Tianjin, China) provided the active study medication and the matching placebo. To safeguard the blinded nature of the study, all bottles with study medication carried a unique identification number. Only patients with a history of stroke or TIA with a stable clinical condition were eligible for participation. Applying the principle of uncertainty, in the early 1990s the clinical investigators excluded all patients with a proven indication or contraindication for blood-pressure-lowering treatment. In contrast to later published noninferiority mega trials,19 we tested the superiority of indapamide vs. placebo using two-sided tests.
In three early trials,4, 5, 6 in which either methyclothiazide combined with deserpidine4 or atenolol5, 6 were compared with placebo, the average reduction in blood pressure ranged from 4.06 to 25.0 mm Hg4 systolic and from 2.95 to 12.3 mm Hg4 diastolic. These three studies4, 5, 6 could not confirm the significant 67% benefit of active treatment (Table 5) on stroke recurrence (P=0.02), as initially reported by Carter in a much smaller trial.3 In 1520 Chinese Perindopril PrOtection Against Recurrent Stroke Study (PROGRESS) patients, active treatment, consisting of indapamide (2.5 mg per day), which in most centers was combined with perindopril (4 mg per day), lowered blood pressure by 14 mm Hg systolic and 6 mm Hg diastolic and reduced stroke recurrence by 55% (95% CI: 40–65%).7, 11, 20 In the Heart Outcomes Prevention Evaluation (HOPE) trial,8 1013 patients with a previous history of cerebrovascular disease were randomized to treatment with ramipril (up to 10 mg daily) or matching placebo, given in addition to unspecified background therapy. Compared with placebo, ramipril reduced blood pressure by 3.1 mm Hg systolic and 1.7 mm Hg diastolic, but the relative risk reduction of 15% in stroke recurrence was not significant (95% CI: −42 to 30%). The Felodipine EVent Reduction study (FEVER) included 2368 Chinese patients with a history of cerebrovascular disease (24.2% of 9800 randomized patients).10 FEVER patients, whose blood pressure on treatment with 12.5 mg of hydrochlorothiazide per day remained in the range of 140–180 mm Hg systolic or 90–100 mm Hg diastolic, were randomized to treatment with extended release felodipine 5 mg per day, or placebo.10 In post-stroke FEVER patients, felodipine reduced blood pressure by 4.0 mm Hg systolic and 1.8 mm Hg diastolic (Figure 4), but the odds ratio for stroke recurrence in patients on felodipine vs. placebo was not significant (0.81; 95% CI: 0.58–1.13). In the PRoFESS trial,1 addition of telmisartan (80 mg daily) to the background treatment in patients with ischemic stroke did not significantly reduce the incidence of recurrent stroke (−5%; 95% CI: −14 to 4%; P=0.23) or of major cardiovascular events (−6%; 95% CI: −13 to 1%; P=0.11) when compared with the placebo treatment.
In our meta-analysis (Figure 4), blood-pressure-lowering treatment across 10 trials (11 groups), including treatment with perindopril only and combination treatment with perindopril and indapamide in the PROGRESS trial,7 reduced the risk of recurrent stroke by 22%. In the trials involving diuretics as a component of therapy,2, 3, 4, 7 the pooled reduction in blood pressure averaged 37%, whereas there was only a 7% reduction in blood pressure in trials using renin system inhibitors.1, 5, 6, 7, 8 As suggested by our meta-regression analysis, the significant heterogeneity (P=0.0003) between diuretics and renin system inhibitors in the prevention of stroke recurrence might be explained by the larger blood pressure reduction that is observed when patients are on treatment regimens that involve diuretics. In vitro and in vivo studies in animals and humans showed that the blood-pressure-lowering action of indapamide not only involves increased natriuresis but inhibition of the contractile responses of vascular smooth muscle cells to vasopressors and adrenergic stimulation as well.16, 18 Diuretics21, 22 and calcium channel blockers22, 23 probably have a small 5–10% benefit beyond blood pressure lowering in the prevention of stroke. Unlike thiazide diuretics, indapamide,18, 24, 25 as well as calcium channel blockers, inhibit the inward current of calcium across cell membranes and reduce intracellular calcium concentrations. In addition to the ensuing vasodilatory effect, lower intraneuronal calcium concentrations protect the ischemic brain.26 Whatever mechanism underlies the benefits of indapamide in the secondary (Figure 4) and the primary27 prevention of stroke, our current meta-analysis does not support the recommendation that prevention of stroke recurrence is a compelling indication for the use of angiotensin-converting enzyme inhibitors.28 Our meta-analysis and PRoFESS also do not support the hypothesis29, 30 that angiotensin receptor blockers are particularly beneficial in the prevention of stroke.
We did not find any heterogeneity in the protection against stroke recurrence among patients with an interval between the qualifying event and randomization below or over 6 months. In an analysis of the PRoFESS trial,1 including only the 1141 strokes that occurred 6 months after randomization, stroke recurrence decreased by 12% (95% CI: 1–22%; P=0.04). The PRoFESS report1 proposed noncompliance with the proportional hazards assumption as the justification for this post-hoc analysis, which was carried out after inspection of the Kaplan–Meier curves (see Figure 1 in reference 1). Significant P-values in the time-stratified analysis were therefore produced after having looked at the data. All outcome analyses involved a time-to-event approach and included all randomized patients.1 Thus, for the results 6 months after randomization, patients who experienced an event earlier were censored at the time of the event and treated in the analysis as if no event had occurred. This approach1 excluded a total of 673 patients, who experienced stroke recurrence within 6 months of randomization. According to our calculations, the odds of stroke recurrence were similar in PRoFESS patients randomized within 10 days of the qualifying event (0.92; 95% CI: 0.81–1.04; n=8087; P=0.19) and in those randomized later (0.93; 95% CI: 0.84–1.03; n=12 201; P=0.18). The reported P-value for interaction was 0.84.1 In the PATS trial, only 64 placebo-treated patients and 85 patients on active treatment were randomized within 10 days of a qualifying cerebrovascular event.
The PATS trial must be interpreted within the context of its limitations. PATS was a large simple trial.17 We did not collect information on previous treatment or on background treatment after randomization. However, in the early 1990s, few Chinese patients with hypertension were on treatment with blood-pressure-lowering drugs. Background treatment was very rarely prescribed during the PATS trial. During the trial, 731 patients randomized to indapamide treatment discontinued their study medication and, therefore, any form of blood-pressure-lowering drug treatment. At the time that the PATS trial was prematurely terminated, 28.1% of randomized patients had been lost to follow-up.
Notwithstanding the above limitations, our findings have implications for health policies in China and possibly other Asian or developing countries. High blood pressure is the predominant underlying risk factor for stroke.31 Increasing the control of hypertension, especially in developing countries where the mortality rate for stroke is over 80%, is of paramount importance. In China, the world's most populous nation, only 44.7% of hypertensive patients are aware of their high blood pressure, only 28.2% are taking antihypertensive medications and only 8.1% manage to control their blood pressure.32 Worldwide, the number of stroke survivors, disabled or not, was estimated to be 62 million in 2005, and this number is projected to rise to 67 and 77 million in 2015 and 2030, respectively.33 The introduction and maintenance of adequate blood-pressure-lowering treatments in stroke survivors still remains to be implemented on a wider scale, particularly in the developing world. Making blood-pressure-lowering drugs available and affordable is a high priority for the secondary as well as the primary prevention of stroke. In China, a country that stands as a model for many developing nations, 79% of rural dwellers and 45% of urban citizens still do not have health insurance.34
In conclusion, blood pressure lowering by the use of a thiazide-like diuretic reduced stroke recurrence and cardiovascular events in normotensive and hypertensive Chinese patients with a history of cerebrovascular disease. As reviewed elsewhere,35 findings from recent trials appear inconsistent with respect to the uniformity in the relationship between cardiovascular benefits and the reduction in blood pressure at all blood pressure ranges, all levels of total cardiovascular risk and with all drug combinations. As highlighted by the current meta-analysis, whether prevention of stroke recurrence depends on drug class, the degree of blood pressure lowering or both, remains to be determined.
Conflict of interest
The authors declare no conflict of interest.
References
Yusuf S, Diener HC, Sacco RL, Cotton D, Ounpuu S, Lawton WA, Palesch Y, Martin RH, Albers GW, Bath P, Bornstein N, Chan BPL, Chen ST, Cunha L, Dahlöf B, De Keyser J, Donnan GA, Estol C, Gorelick P, Gu V, Hermansson K, Hilbrich L, Kaste M, Lu C, Machnig T, Pais P, Roberts R, Skvortsova V, Teal P, Toni D, VanderMaelen C, Voigt T, Weber M, Yoon BW, for the PRoFESS Study Group. Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med 2008; 359: 1225–1237.
PATS Collaborative Group. Post-stroke antihypertensive treatment study. A preliminary result. Chin Med J 1995; 108: 710–717.
Carter AB . Hypotensive therapy in stroke survivors. Lancet 1970; 1: 485–489.
Hypertension-Stroke Cooperative Study Group. Effect of antihypertensive treatment on stroke recurrence. JAMA 1974; 229: 409–418.
The Dutch TIA Trial Study Group. Trial of secondary prevention with atenolol after transient ischemic attack or nondisabling ischemic stroke. Stroke 1993; 24: 543–548.
Eriksson S, Olofsson BO, Wester PO, for the TEST study group. Atenolol in secondary prevention after stroke. Cerebrovasc Dis 1995; 5: 21–25.
PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet 2001; 358: 1033–1041.
Bosch J, Yusuf S, Pogue J, Sleight P, Lonn E, Rangoonwala B, Davies R, Ostergren J, Probstfield J, on behalf of the HOPE Investigators. Use of ramipril in preventing stroke: double blind randomised trial. BMJ 2002; 324: 1–5; full text available at http://bmj.com/cgi/content/full/324/7339/699.
Trenkwalder P, Elmfeldt D, Hofman A, Lithell H, Olofsson B, Papademetriou V, Skoog I, Zanchetti A . The Study on COgnition and Prognosis in the Elderly (SCOPE)—major CV events and stroke in subgroups of patients. Blood Press 2005; 14: 31–37.
Liu L, Zhao Y, Liu G, Li W, Zhang X, Zanchetti A, for the FEVER Study Group. The Felodipine Event Reduction (FEVER) Study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens 2005; 23: 2157–2172.
PROGRESS Management Committee. PROGRESS—Perindopril Protection Against Recurrent Stroke Study: characteristics of the study population at baseline. J Hypertens 1999; 17: 1647–1655.
The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med 2000; 342: 145–153.
Lithell H, Hansson L, Skoog I, Elmfeldt D, Hofman A, Olofsson B, Trenkwalder P, Zanchetti A, for the SCOPE Study Group. The study on cognition and prognosis in the elderly (SCOPE). Principal results of a randomised double-blind intervention trial. J Hypertens 2003; 21: 875–886.
Holmer SR, Hense HW, Danser AHJ, Mayer B, Riegger GAJ, Schunkert H . Adrenergic blockers lower renin in patients treated with ACE inhibitors and diuretics. Heart 1998; 80: 45–48.
Staessen JA, Li Y, Richart T . Oral renin inhibitors. Lancet 2006; 346: 1449–1456.
Chaffman M, Heel RC, Brogden RN, Speight TM, Avery GS . Indapamide. A review of its pharmacodynamic properties and therapeutic efficacy in hypertension. Drugs 1984; 28: 189–235.
Yusuf S, Collins R, Peto R . Why do we need large, simple randomized trials? Stat Med 1984; 3: 409–422.
Campbell DB, Brackman F . Cardiovascular protective properties of indapamide. Am J Cardiol 1990; 65: 11H–127H.
The ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358: 1547–1559.
Liu L, Gong L, Wang W, for Blood Pressure Lowering to Prevent Recurrent Stroke Study Group. Effects of blood pressure lowering treatment in patients with cerebrovascular disease—a large scale, randomized, placebo controlled trial. Chin J Cardiol 2005; 33: 613–617.
Messerli FH, Grossman E, Lever AF . Do thiazide diuretics confer specific protection against strokes? Arch Intern Med 2003; 163: 2557–2560.
Blood Pressure Lowering Treatment Trialists Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003; 362: 1527–1535.
Verdecchia P, Reboldi G, Angeli F, Gattobigio R, Bentivoglio M, Thijs L, Staessen JA, Porcellati C . Angiotensin-converting enzyme inhibitors and calcium channel blockers for coronary heart disease and stroke prevention. Hypertension 2005; 46: 386–392.
Mironneau J, Savineau JP, Mironneau C . Compared effects of indapamide, hydrochlorothiazide and chlorthalidone on electrical and mechanical activities in vascular smooth muscle. Eur J Pharmacol 1981; 75: 109–113.
Mironneau J, Savineau JP, Mironneau C . Effect of indapamide on the electromechanical properties of rat myometrium and rat portal vein. J Pharmacol Exp Ther 1986; 236: 519–525.
Lee JM, Zipfel GJ, Choi DW . The changing landscape of ischaemic brain injury mechanisms. Nature 1999; 399 (Suppl): A7–A14.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, Stoyanovski V, Antikainen R, Nikitin Y, Anderson C, Belhani A, Forette F, Rajkumar C, Thijs L, Banya W, Bulpitt CJ, for the HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358: 1887–1898.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, Jones DW, Materson BJ, Oparil S, Wright Jr JT, Roccella EJ . Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003; 42: 1206–1252.
Dalmay F, Mazouz H, Allard J, Pesteil F, Achard JM, Fournier JM . Non-AT1-receptor mediated protective effect of angiotensin against acute ischaemic stroke in the gerbil. J Renin Angiotensin Aldosterone Syst 2001; 2: 103–106.
Fournier A, Oprisiu R, Andrejak M, Godefroy O, Rosa A, Achard JM . Age-adjusted stroke incidence increase: could angiotensin AT1 receptor antagonists enhance stroke prevention? Stroke 2002; 33: 881–882.
Zhang H, Thijs L, Staessen JA . Blood pressure lowering for the primary and secondary prevention of stroke. Hypertension 2006; 48: 187–195.
Gu D, Reynolds K, Wu X, Chen J, Duan X, Muntner P, Huang G, Reynolds RF, Su S, Whelton PK, He J . Prevalence, awareness, treatment, and control of hypertension in China. Hypertension 2002; 40: 920–927.
Strong K, Mathers C, Bonita R . Preventing stroke: saving lives around the world. Lancet Neurol 2007; 6: 182–187.
Wang L, Kong L, Wu F, Bai Y, Burton R . Chronic Diseases 4. Preventing chronic diseases in China. Lancet 2005; 366: 1821–1824.
Zanchetti A, Mancia G, Black HR, Oparil S, Waeber B, Schmieder RE, Bakris GL, Messerli FH, Kjeldsen SE, Ruilope LM . Facts and fallacies of blood pressure control in recent trials: implications in the management of patients with hypertension. J Hypertens 2009; 27: 673–679.
Acknowledgements
L Liu and L Gong coordinated the PATS trial; Z Wang, Y Zhang and J Wang maintained the database and carried out statistical analyses; L Thijs supervised SAS programming and the statistical analyses; and Z Wang and JA Staessen wrote the first draft of this paper. All authors commented on this paper and approved the final version. The Chinese Ministry of Health (Xicheng District, Beijing, China), the Chinese World Bank Office (China World Trade Center, Beijing, China) and Lisheng Pharmaceutical Company (Tianjin, China) supported the Post-stroke Antihypertensive Treatment Study. The Bilateral Scientific and Technological Cooperation between China and Flanders (BIL02/10) supported the fellowship of J Wang (Leuven, Belgium). The European Union (Grants IC15-CT98-0329-EPOGH, LSHM-CT-2006-037093 InGenious HyperCare and HEALTH-F4-2007-201550 HyperGenes), the Fonds voor Wetenschappelijk Onderzoek Vlaanderen, the Ministry of the Flemish Community, Brussels, Belgium (Grants G.0453.05 and G.0575.06) and the University of Leuven, Belgium (OT/00/25 and OT/05/49) provided support to the Studies Coordinating Centre. Richard Peto (Clinical Trial Service and Epidemiological Studies Unit, University of Oxford, Oxford, UK) helped in designing the trial. Tom Richart, MD, MBE made the graphics. The authors gratefully acknowledge the secretarial assistance of Sandra Covens and Ya Zhu (Studies Coordinating Centre, University of Leuven, Leuven, Belgium).
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix
Appendix
PATS Collaborating Group
Trial Coordinators: Liu Lisheng and Gong Lansheng; Data Monitoring Committee: Liu Guozhang, Wang Jiguang, Wang Xianyan and Fang Weiqing; Drug Committee: Liu Guozhang, Wang Jiguang and Zhang Peijie; Ethics Committee: Liu Lisheng and Gong Lansheng; Steering Committee: Liu Lisheng, Liu Guozhang, Hong Zhaoguang, Pu Shouyue, Qi Wenhang, Wang Lihui, Wang Xinde and Wang Zitong.
Participating Centers
Fuwai Hospital (http://www.fuwaihospital.org); Capital Iron and Steel Complex Hospital (http://www.sgyy.com.cn); 301 Hospital, People's Liberation Army (http://www.301hospital.com.cn); 514 Hospital, People's Liberation Army; 361 Hospital, People's Liberation Army; 292 Hospital, People's Liberation Army; Nanfang Hospital of Guanszhou (http://www.nfyy.com); The Affiliated Hospital of Guiyang Medical College of Guiyang (http://www.gmcah.com); Hebei Academy of Medical Sciences of Shijiazhuang; Second Hospital of Baoding; Dongkuang Hospital of Tangshan; Fengrun Hospital of Traditional Chinese Medicine; Qinhuangdao, Seaport Hospital; Beidaihe Hospital of Qinhuangdao; First Hospital of Daqing (http://www.first-hospital.com); First Affiliated Hospital of Henan Medical University of Zhengzhou (http://zdyfy.com); Henan Academy of Traditional Chinese Medicine Zhengzhou (http://www.hntcm.com); Prefecture Hospital of Zumadian; City Hospital of Zumadian; Prefecture Hospital of Nanyang; Affiliated Hospital of Nanyang Medical School; First Hospital of Wuhan Iron and Steel Complex, Wuhan; First Affiliated Hospital of Hunan Medical University of Changsha (http://www.xiangya.com.cn); Affiliated Hospital of Nanjing Medical College (http://www.jsph.net); Affiliated Hospital of Zhenjiang Medical College; City Hospital of Yancheng; Affiliated Hospital of Xuzhou Medical College (http://www.xzmc.edu.cn); Affiliated Hospital of Gannan Medical College (http://www.gyfy.com.cn); Affiliated Hospital of Jilin Medical College; Second Affiliated Hospital of Dalian Medical College (http://www.dy2y.com); Dalian Cardio Cerebrovascular Institute; Changdian Hospital of Anshan; Central Hospital of Benxi (http://bxzxyy.china315.com); General Hospital of Benxi Iron and Steel Complex; Fushun Steel Plant Hospital; Yuanbao Hospital of Dandong; Railway Hospital of Xining; Shandong Academy of Medical Sciences of Jinan (http://www.sdstcc.gov.cn); Huimin Prefecture Hospital; Mine Affairs Hospital of Yangquan; Tianjin Cardiovascular Institute; Shanghai Institute of Hypertension (http://www.china-sih.com); Shanghai Cardiovascular Institute (http://www.zs-hospital.sh.cn); City Hospital of Ningbo (http://www.nbdyyy.com); Guanganmen Hospital (http://www.gamhospital.ac.cn).
Rights and permissions
About this article
Cite this article
Liu, L., Wang, Z., Gong, L. et al. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res 32, 1032–1040 (2009). https://doi.org/10.1038/hr.2009.139
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.139
Keywords
This article is cited by
-
Intensive or standard blood pressure control in patients with a history of ischemic stroke: RESPECT post hoc analysis
Hypertension Research (2022)
-
Effectiveness of Perindopril/Indapamide Single-Pill Combination in Uncontrolled Patients with Hypertension: A Pooled Analysis of the FORTISSIMO, FORSAGE, ACES and PICASSO Observational Studies
Advances in Therapy (2021)
-
Ambulatory blood pressure monitoring on admission in survivors of recent stroke entering inpatient rehabilitation
Journal of Human Hypertension (2020)
-
Nurse-led, telephone-based secondary preventive follow-up benefits stroke/TIA patients with low education: a randomized controlled trial sub-study
Trials (2019)
-
2018 Korean society of hypertension guidelines for the management of hypertension: part III-hypertension in special situations
Clinical Hypertension (2019)